
Figure 24
You’d like to see a post operative picture somewhat like that. [see Figure 24] At least in our hands, that’s the procedure.
With any surgery there are always some risks. There’s a risk of leaking spinal fluid beyond the graft where you’re sewing in a water bag, basically. You can always have a risk of wound infection, meningitis, pain at the occipital nerves which run off to the side in the back of your head. The worst thing obviously would be a neurological deficit or stroke. And there are some other general medical risks to the surgery, so we have to keep those in mind and let me briefly run through just a few cases.
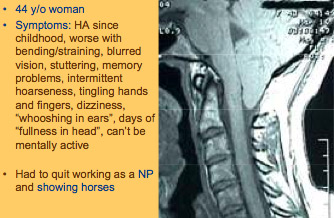
Figure 25
Here’s a 44 year old woman, [see Figure 25] she’s had headaches since childhood. They’re worse with bending, straining. She complains of blurred vision and stuttering, memory problems, intermittent hoarseness, tingling of the hands, dizziness, whooshing in her ears, fullness in her head and can’t be mentally active. She was advised to give up her nurse practitioner job. She did that, then she was advised that she had Chiari and that what she should do is give up her hobbies as well, which in her case was showing horses. At that point she took her life under her own hands and started trying to find out and learn about this. As you can see, a fairly pronounced herniation of the tonsils. In her case this is the preoperative and this is the postoperative with adding the graft. Not everyone does excellently. Let me repeat that and I’m sure we’ll talk about that throughout the meeting but she was obviously very pleased. Did not go back to nurse practitioning, but did not quit horse riding.

Figure 26
Here’s another, [see Figure 26] and this is just to point out, as Dr. Milhorat and others have pointed out, that up to about 1/4 of people with Chiari malformation, the symptoms will be trigger by a trauma and it doesn’t have to be a high speed motor vehicle collision. In this case it was a trampoline accident; this is when the extreme headaches began. Fatigue, distant looking eyes, heart palpitations, shooting pain, shortness of breath, poor sleep, anxiety, chest pain; a variety of symptoms. This is her obstruction in this area here, this is her postoperatively. Other than some occasional occipital pain, was doing quite well.

Figure 27
A young man, thick bone, [see Figure 27] sort of a boney anomaly if you will, very pointed, crowded tonsils. Here’s your foramen magnum- laughter almost causes him to pass out. These are some of the weightful centers – if you will – reticular activating centers – are in those areas that help control consciousness and he was probably impacting that area so tightly, feeling possibly loss of consciousness on that mechanism. Postoperatively this is what you’d like to see. [see Figure 28]
But on the other hand, let me say not everyone does well and there’s a lot of work to be done. Dr. Meuller and I, in the Neurosurgical Focus last year, published 112 patients whom we did an outcome study and I think you’ll hear more about that today, where they had a 6 or 8 page questionnaire before surgery and then a year after. We found 84% of people seemed to have very good outcome following this. Fortunately a lot of people can improve but not everyone. Now I think as you’ll also hear some of those people that did not improve also point to things like a back fusion surgery or other medical problems they had in that coming year. So it’s a little difficult to tease out exactly how people do following Chiari surgery and that’s going to be one, I think.

Figure 28
In our experience, to summarize, in our clinic we’ve focused quite a lot in keeping the complications as low as possible and I think we’ve been able to do that. I think the challenge, at least before us, and I think maybe others, is how can we better define who truly needs the operation and how can we improve our outcome? With that I thank you very much for the opportunity.
John Oró
Medical Director,
The Neurosurgery Center of Colorado
Founder Chiari Treatment Center
Aurora, Colorado

