2025 Conference Program
2025 Conference Program
PROGRAM & SPEAKERS
The 2025 official speakers and program times are currently subject to change. View speakers here (subject to change)
Monday, July 21, 2025
- Evening opening reception dinner & entertainment
Tuesday, July 22, 2025
- Breakfast
- Support group meeting
- Morning lectures & Q&A Panels
- Lunch break
- Afternoon lectures & Q&A Panels
- Evening outing (TBD)
Wednesday, July, 23, 2025
- Breakfast
- Support group meeting
- Morning lectures & Q&A Panels
- Lunch break
- Afternoon lectures & Q&A Panels
- Free evening (enjoy your time in Iowa City)
Thursday, July, 24, 2025
- Breakfast
- Support group meeting
- Morning lectures & Q&A Panels
- Lunch break
- Afternoon lectures & Q&A Panels
- Afternoon closing reception
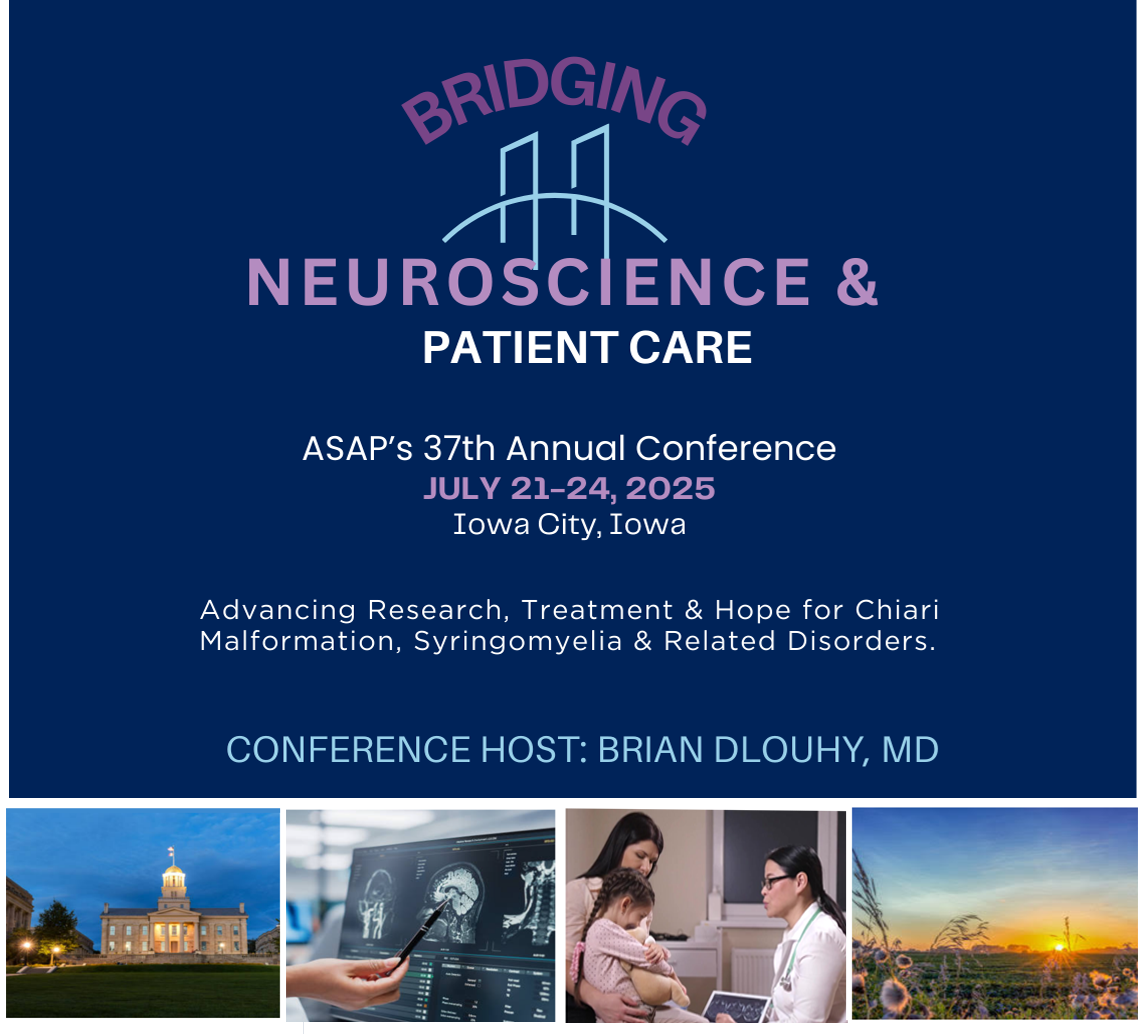
Topics
- Arachnoiditis
- Chiari (2)
- Ehlers-Danlos Syndrome
- Treatment/Surgery
- MCAS
- Neurotechnology
- Intracranial Hypotension
- CSF Leaks
- Genetics
- Scoliosis
- Pediatrics
- Pain/Headaches
- Syringomyelia
- Pediatric Scoliosis
We are thrilled to welcome an outstanding lineup of speakers to the 2025 ASAP Annual Conference. This year’s presenters represent a dynamic cross-section of thought leaders, innovators, and practitioners from across the field, each bringing unique perspectives, expertise, and insights to our shared mission. As we gather to explore new challenges, celebrate progress, and envision the future, these distinguished speakers will help guide the conversation and inspire meaningful action.
Watch for more interesting topics and speakers.
2025 Conference Speakers
 Synopsis: Discuss the numerous craniocervical bony and ligamentous abnormalities associated with Chiari malformation and their treatment strategies from the Iowa database.
Synopsis: Discuss the numerous craniocervical bony and ligamentous abnormalities associated with Chiari malformation and their treatment strategies from the Iowa database.
ASAP 2025 Conference Host: Brian J Dlouhy, MD
About Dr Dlouhy: Dr. Brian Dlouhy is a pediatric and adult neurosurgeon at the University of Iowa Hospitals & Clinics and University of Iowa Children’s Hospital in Iowa City, Iowa. He completed his neurosurgery residency at the University of Iowa working extensively under Dr. Arnold Menezes. He now works side by side with Dr. Arnold Menezes treating all disorders of the craniovertebral junction (CVJ) in children and adults. He also has an active research program studying the pathophysiology of Chiari I malformation and other conditions of the CVJ.
 Synopsis: Arachnoiditis is an overgrowth of fibrous tissue within the spinal subarachnoid space that follows inflammation within the spinal subarachnoid space. Each year, about 25,000 people develop arachnoiditis, mainly in North and South America, Asia, and Europe. The neurological symptoms, signs, and prognosis of patients with arachnoiditis are variable and unpredictable. The excess fibrous tissue can tether the spinal cord to the adjacent dura and obstruct spinal cerebrospinal fluid (CSF) flow. Spinal cord tethering reduces spinal cord motion, blood supply, and function. Scarring that obstructs spinal CSF pathways may result in syrinx formation.
Synopsis: Arachnoiditis is an overgrowth of fibrous tissue within the spinal subarachnoid space that follows inflammation within the spinal subarachnoid space. Each year, about 25,000 people develop arachnoiditis, mainly in North and South America, Asia, and Europe. The neurological symptoms, signs, and prognosis of patients with arachnoiditis are variable and unpredictable. The excess fibrous tissue can tether the spinal cord to the adjacent dura and obstruct spinal cerebrospinal fluid (CSF) flow. Spinal cord tethering reduces spinal cord motion, blood supply, and function. Scarring that obstructs spinal CSF pathways may result in syrinx formation.
Various inflammatory conditions and agents can cause arachnoiditis and influence its anatomical site and scope. For example, meningitis is a condition that extends broadly through the intracranial and intraspinal subarachnoid spaces and usually causes extensive arachnoiditis affecting four or more vertebral segments. On the other hand, spinal trauma typically involves one or two adjacent spinal segments and produces focal arachnoiditis only at those vertebral segments. The disease course of patients with arachnoiditis varies. Patients with extensive arachnoiditis generally have a worse prognosis than those with focal arachnoiditis. Medical practitioners and researchers do not understand the expected course of arachnoiditis well enough to design trials that test new treatments. A better understanding of arachnoiditis’s natural history and disease mechanisms may lead to clinical trials of new drugs and surgical treatments that can effectively reduce subarachnoid inflammation and fibrosis and improve the treatment of patients with arachnoiditis.
About Dr Heiss: Dr John D. Heiss, is a Senior Clinician, the Head of the Clinical Unit of the Surgical Neurology Branch, and Program Director of the Neurological Surgery Residency Training Program at the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH) in Bethesda, Maryland. He is actively involved in clinical and translational research to improve the understanding and treatment of Chiari I malformation, syringomyelia, pain, brain tumors, and Parkinson’s disease. He is board-certified in neurological surgery and an expert in supervising and conducting clinical trials for CNS disorders. Dr. Heiss received his B.S. in Biomedical Sciences and M.D. from the University of Michigan. In addition, he completed his surgical internship and residency in neurosurgery at the University of Cincinnati College of Medicine. Before joining NINDS, Dr. Heiss was Co-Director of the Neuroscience Intensive Care Unit at the University of Cincinnati.
About Dr. Iskandar: Dr. Bermans Iskandar is Professor of Neurosurgery and Pediatrics, and Director of the Pediatric Neurosurgery program at the University of Wisconsin Hospital and Clinics. His clinical interests include neuro-endoscopy, brachial plexus reconstruction, and surgery of congenital CNS malformations, especially hydrocephalus, Chiari malformations, and syringomyelia. Led by Dr. Iskandar, the Wisconsin Hydrocephalus Group (WHP) of engineers, physicists, neurologists, and neurosurgeons aims to determine the etiology of ventricular shunt malfunction and optimize the devices used to treat it. As well, Dr. Iskandar directs a translational research laboratory that has uncovered an important link between folate metabolism, epigenetic influences, and axonal regeneration after central nervous system injury. Dr. Iskandar has recently concluded his service as Chair of the AANS/CNS Section on Pediatric Neurosurgery, and Chair of the American Board of Pediatric Neurological Surgery.
 Jamila Hamdan: Lead Genetic Counseling Assistant – Medical Genetics
Jamila Hamdan: Lead Genetic Counseling Assistant – Medical Genetics
 Synopsis: Myodural bridges (MDBs) provide spinal cord support during head and neck movement, and regulate cerebrospinal fluid (CSF) flow at the craniocervical junction (CCJ). Previous studies have associated abnormal spinal cord motion with MDB structural collagen abnormalities in patients with hypermobile Ehlers-Danlos Syndrome (hEDS) and Chiari malformation (CM1). These findings may translate to CM1 patients more broadly. The presentation will discuss the current research that aims to characterize MDBs in CM1 via dynamic CCJ ultrasound (US) and tissue biomechanical analysis and discuss their potential role in the pathophysiology of Chiari malformation.
Synopsis: Myodural bridges (MDBs) provide spinal cord support during head and neck movement, and regulate cerebrospinal fluid (CSF) flow at the craniocervical junction (CCJ). Previous studies have associated abnormal spinal cord motion with MDB structural collagen abnormalities in patients with hypermobile Ehlers-Danlos Syndrome (hEDS) and Chiari malformation (CM1). These findings may translate to CM1 patients more broadly. The presentation will discuss the current research that aims to characterize MDBs in CM1 via dynamic CCJ ultrasound (US) and tissue biomechanical analysis and discuss their potential role in the pathophysiology of Chiari malformation.
About Dr Klinge: Dr. Petra Klinge serves as an internationally renowned clinician for diagnosing and neurosurgical treatment of patients with CSF disorders working on the unifying concept of cognitive problems related pathology in Hydrocephalus of aging and pediatric patients. Her practice also includes patients with associated developmental Cerebrospinal fluid disorders, such as spina bifida, Chiari malformation, tethered cord, patients with connective tissue disorders and associated spinal fluid disorders including syringomyelia and occult tethered cord syndrome. Her research focuses on the pathophysiology and diagnosis of tethered cord and on establishing criteria and clinical biomarkers for surgical intervention in tethered cord syndromes (1-5).
In collaboration with neuroradiology in her practice at Rhode Island Hospital and the Carney-Institute and the department of bio-engineering at the Brown Medical School she develops pioneering and novel clinical and in-vivo diagnostics and pathological studies to improve the management and validation of those conditions.
In the past 2 years, Dr. Klinge has also collaborated with the University of Akron Conquer Chiari Research Center, founded by the Department of Psychology and the Department of Biomedical Engineering on the implications of ageing in Chiari as well as identifying cognitive and imaging biomarkers to support the biodynamic concept of the failure of Cerebrospinal fluid regulation at the base of the skull in adult Chiari malformation. Her research has focused on the failure of “Myodural bridges” and defunct collagen that supports the aspects of CSF circulatory failure at the base of the skull in various conditions including Chiari associated with connective tissue disease and she works on the novel concept of a “Spinal cord motion disorder” that might explain and support occult neurosurgical pathologies associated with impaired CSF regulation and tethering of the spinal cord and brain stem. She had been appointed by the National Academy of Sciences and has served in 2022 in a committee to establish disability criteria for the neurological conditions in patients with Ehlers-Danlos-Syndrome and Marfan Syndrome as an nationally acknowledged expert for spinal cord disorders and tethered cord syndrome. Selected Heritable Disorders of Connective Tissue and Disability | National Academies.
 Synopsis: We will discuss an analysis of a patient operated on by Wilder Penfield in 1938. The preoperative diagnosis was a CP angle tumor, and perhaps the search for the lesion led to an extensive suboccipital craniectomy that became the standard for Chiari. Dr Bucy had a similar experience with another patient shortly after. Besides describing the cases, I discuss the significance of case reports in the evidence about optimal treatments for Chiari.
Synopsis: We will discuss an analysis of a patient operated on by Wilder Penfield in 1938. The preoperative diagnosis was a CP angle tumor, and perhaps the search for the lesion led to an extensive suboccipital craniectomy that became the standard for Chiari. Dr Bucy had a similar experience with another patient shortly after. Besides describing the cases, I discuss the significance of case reports in the evidence about optimal treatments for Chiari.
About Dr Lazareff: Emeritus Professor of Neurosurgery, Department of Neurosurgery. David Geffen School of Medicine. University of California, Los Angeles. Clinical and research interest in congenital malformations of the Central Nervous System. Currently involved in studying barriers to care for congenital diseases of the nervous system.
 Synopsis: Pending
Synopsis: Pending
About Dr Maitland:
Anne L. Maitland, MD, PhD is
- the Director, the Ehlers Danlos Syndrome Institute, at Medical University of South Carolina, and
- an Associate Professor in the Department of Medicine, Division of Rheumatology at the Medical University of South Carolina
Her career has long been driven by curiosity about the neuro-immune axis and its dysregulation in disease. She was introduced to the spectrum of neuroimmune dysregulation, as she witnessed the HIV and asthma epidemics unfold in her hometown, in the 1980s. Nowadays, Long COVID exemplifies acquired neuro-immune dysregulation, which follows infection by SARS CoV-2 and impacts 7% of the US population; and, children as well as adults with connective tissue disorders, such as Ehlers-Danlos Syndromes (EDS), face neurodevelopmental challenges and heightened sensitivity to environmental exposures, which reflect chronic dysregulation of the autonomic nervous and immune systems, respectively.
In collaboration with Drs. Norris, Gensemer and Patel, Ehlers-Danlos Syndrome Institute (EDSI) will become a model of innovative care for complex medical disorders, amidst of sea of siloed healthcare.
Dr. Maitland serves on committees, addressing mast cell activation disease (MCAD), Health Care Disparities and Integrative Medicine of the American Academy of Allergy, Asthma and Immunology. She also serves on the scientific faculty for the Mast Cell Disease Society, the Ehlers-Danlos International Consortium and the Chiari-Syringomyelia Foundation.
Synopsis: Pending

After graduating from the University of Cincinnati College of Medicine Dr. Martin completed a residency in internal medicine, followed by a fellowship in general internal medicine at UC. Dr. Martin was Chief Resident of the Department of Internal Medicine during his fellowship at UC.
 Synopsis: Chiari malformation and syringomyelia are complex problems that require thoughtful evaluation and treatment. When they do – there are special considerations, treatment plans, and follow up should occur. In most cases, further investigation is needed. Furthermore there is a well-known relationship between Chiari malformation and thoracolumbar scoliosis. The incidence of scoliosis is 2 to 4% in the general population but may be as high as 30% in patients with Chiari malformation type 1 and as high as 70% with spinal cord syrinx. In this presentation, we will discuss the relationship between chiari malformation and scoliosis and discuss the most up to date evidence identifying at risk patients and how we diagnose and treat patients who have these diagnoses.
Synopsis: Chiari malformation and syringomyelia are complex problems that require thoughtful evaluation and treatment. When they do – there are special considerations, treatment plans, and follow up should occur. In most cases, further investigation is needed. Furthermore there is a well-known relationship between Chiari malformation and thoracolumbar scoliosis. The incidence of scoliosis is 2 to 4% in the general population but may be as high as 30% in patients with Chiari malformation type 1 and as high as 70% with spinal cord syrinx. In this presentation, we will discuss the relationship between chiari malformation and scoliosis and discuss the most up to date evidence identifying at risk patients and how we diagnose and treat patients who have these diagnoses.
About Dr Ravindra: Dr. Vijay Ravindra is a board certified adult and pediatric neurosurgeon and active duty Naval Officer currently stationed at Naval Medical Center San Diego and affiliated with Rady Children’s Hospital. He completed his neurosurgery training at the University of Utah where he worked closely with Dr. Douglas Brockmeyer. He completed his pediatric neurosurgery fellowship at Texas Children’s Hospital – Baylor College of Medicine. His clinical interests include disorders of the pediatric spinal column, in particular the craniocervical junction and scoliosis. He is actively studying tissue properties of the CCJ in children with Chiari malformations.
About Dr Reynolds: Dr. Rebecca Reynolds is a pediatric neurosurgeon and assistant professor here at the University of Iowa. Her interests lie in global health and differences and disparities in treatment. She has a fantastic presentation on spina bifida in children in Zambia, Africa. This talk would have implications for tethered cord and delay in treatment. Moreover, in general, it’s a very interesting side of global medicine that we do not hear about in the United States very often. She’s fantastic and I think the audience would really appreciate this refreshing unique talk.
Synopsis: Pending
 Samantha Schutt is a registered nurse practitioner at the University of Iowa and has for many years seen and treated our hypermobile and EDS patients. She is truly an expert in the field. As you know, there does appear to be a strong connection between EDS/hypermobility and some Chiari patients.
Samantha Schutt is a registered nurse practitioner at the University of Iowa and has for many years seen and treated our hypermobile and EDS patients. She is truly an expert in the field. As you know, there does appear to be a strong connection between EDS/hypermobility and some Chiari patients.
About Dr Weinstein: Stuart L. Weinstein, MD, is a pediatric orthopedic surgeon who specializes in spinal deformities and hip problems. Weinstein received his medical education and training at the University of Iowa.
His research over the past 40 years has been focused on the natural history and long-term outcomes of pediatric orthopedic conditions, primarily spinal deformities and hip disorders. This research has established the evidence base for the treatment of children with these conditions used around the world. Much of this research has been funded by the National Institute of Health and the Orthopedic Research and Education Foundation and has resulted in over 270 publications in such journals as the New England Journal of Medicine, the Journal of the American Medical Association, and The Lancet.
Weinstein has received many awards over the years for his outstanding work including the State of Iowa Board of Regents Award, the AOA Distinguished Contributions to Orthopedics Award, the Ernest O. Theilen Clinical Teaching and Service Award and the Carver College of Medicine Distinguished Mentor Award. He has also received two Kappa Delta/OREF awards for Outstanding Orthopedic Clinical Research, the highest research awards in Orthopedic Surgery.
Weinstein has been honored for his contributions to Orthopedic Surgery by honorary memberships in National Orthopedic Associations around the world including Australia, New Zealand, Germany, Great Britain, Thailand, China, Portugal, Europe (EFORT), and Argentina. In 2007, he was made a Fellow of the Royal College of Surgeons of England.
Weinstein is past president of the American Academy of Orthopedic Surgeons and the American Orthopedic Association, the American Board of Orthopedic Surgery, and the Pediatric Orthopedic Society of North America.
About Dr Zanaty: Dr. Zanaty is a skull base/endovascular/vascular neurosurgeon and an assistant professor here at the University of Iowa. As you know, intracranial hypotension is challenging to treat. In the last couple years, novel management strategies have emerged. Dr. Zanaty has developed quite a series of patients treating this complicated condition. I believe the patients would be quite interested in this talk.
 Synopsis: In this talk, we will explore the integration of advanced imaging technologies with AI to enhance the diagnosis of brain diseases and predict treatment outcomes. Highlighting recent advancements, we will demonstrate how advanced imaging techniques reveal hidden brain dynamics in patients with Chiari Malformation. We will elucidate how AI-driven imaging analysis improves diagnostic accuracy and helps identify high-risk patients. Additionally, we will discuss the implications of these innovations on patient care, treatment optimization, and quality of life.
Synopsis: In this talk, we will explore the integration of advanced imaging technologies with AI to enhance the diagnosis of brain diseases and predict treatment outcomes. Highlighting recent advancements, we will demonstrate how advanced imaging techniques reveal hidden brain dynamics in patients with Chiari Malformation. We will elucidate how AI-driven imaging analysis improves diagnostic accuracy and helps identify high-risk patients. Additionally, we will discuss the implications of these innovations on patient care, treatment optimization, and quality of life.
About Dr Zhao: Dr. Moss Zhao is an Instructor in the Department of Neurosurgery at Stanford University. He develops cutting-edge and clinically viable imaging technologies to improve the diagnosis and treatment of cerebrovascular diseases across the lifespan. His specific areas of expertise include physiological modeling, image analysis, and artificial intelligence. Dr. Zhao’s scientific contributions aim to significantly improve the early detection of neurological disorders and optimize patient selection in neurosurgical procedures and clinical trials.
Dr. Zhao graduated from University of Oxford. Recently, he received the prestigious Career Development Award from the American Heart and Stroke Association to propel his career as an independent investigator. Dr. Zhao is passionate about science communication and community-engaged research. His science podcasts have been downloaded over 10,000 times in more than 20 countries.
About Dr Zhorne: Leah Zhorne, MD is a general child neurologist with a special clinical interest in headache disorders. She is passionate about improving the quality of patient care in her role as director of the comprehensive headache clinic and in the neurocritical care follow up clinic. She also participates in clinical research, serving as the site PI for the International Pediatric Stroke Study, and as a site sub-investigator in a Gaucher Type 3 Disease clinical trial. Dr. Zhorne also has a special interest in resident education. In her role as Program Director, she continually works to adapt and update the child neurology resident experience to fit the ever-changing needs of our learners.